A D V A N C E D M A T E R I A L S & P R O C E S S E S | J U L Y / A U G U S T 2 0 1 6
2 0
(Fig. 3). Wall thicknesses down to
approximately 0.5 mm are possible and
implants are typically sterilized with
ethylene oxide prior to implantation.
MECHANICAL PROPERTIES
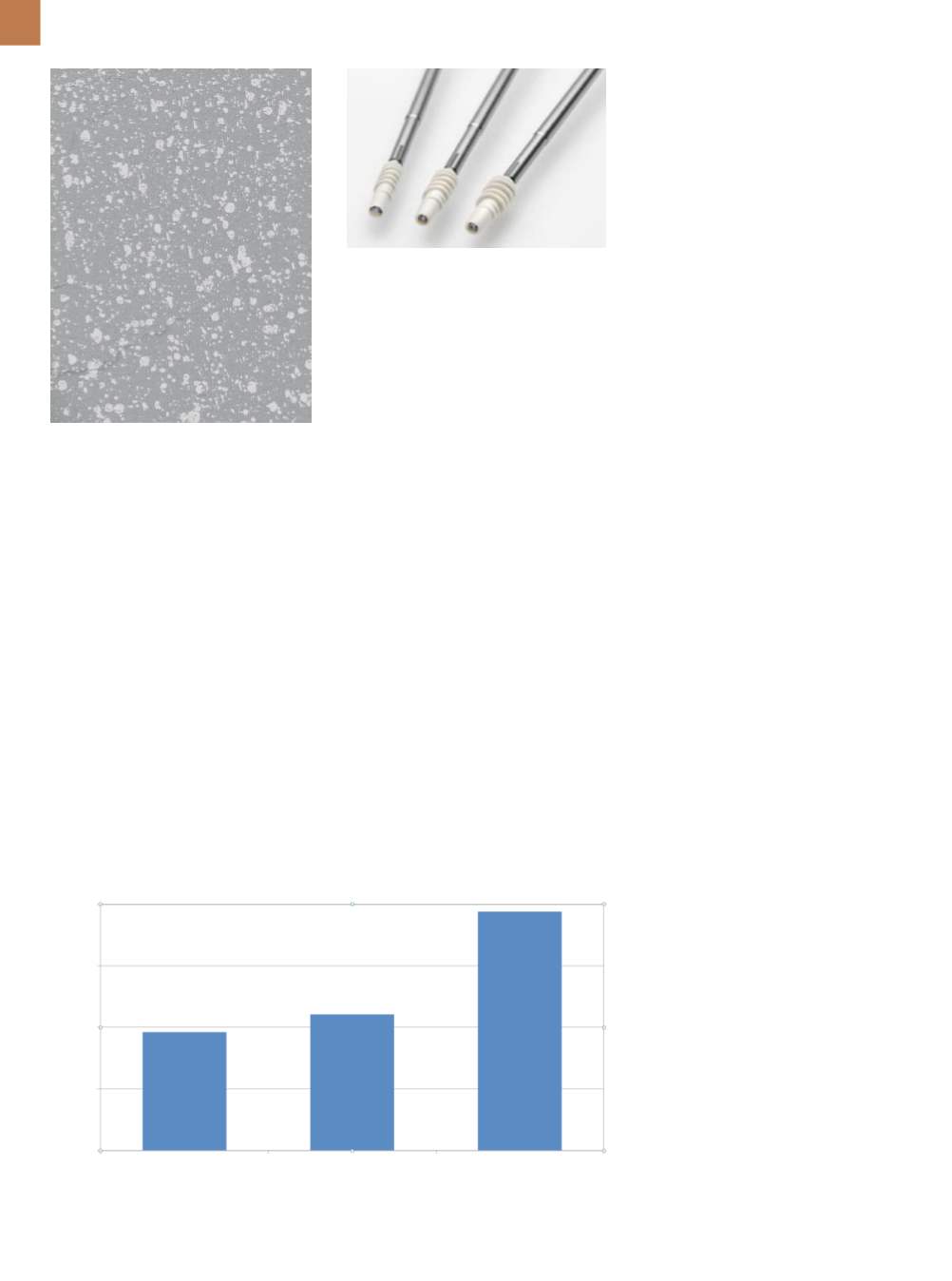
For many orthopedic sports med-
icine applications, the implant’s me-
chanical properties are critical both
immediately after surgery and for the
entire healing period. After the pa-
tient is fully healed, implants should
generally no longer be load bearing.
With BR, adding the bioceramic filler
compromises the inherent strength
of the parent polymer, but not to an
unusable degree. For example, suture
anchors made from BR are rough-
ly 87% of the strength of the same
size suture anchors made from PEEK
(Fig. 4). However, in internal tests,
the tensile modulus is higher for BR
(2.6 GPa) compared to PLLA (2.0 GPa).
In addition to decreasing strength
and increasing modulus,
β
–TCP af-
fects ductility, as might be expected.
Interestingly, internal testing shows
a significant improvement in ductility
as the material is brought from room
temperature to body temperature. In
fact, the engineering strain at fracture
nearly doubles to approximately 9%
over the course of this 14°C tempera-
ture increase. Over the same tempera-
ture rise, maximum stress drops from
72.4 to 53.8 MPa (Fig. 5).
PRECLINICAL STUDY
Despite a long history of clini-
cal use for all three components of BR
(
β
–TCP, PLLA, and PGA), a preclinical
study was performed on the specific
blend of these components in BR. A
femoral transcortical model using Bea-
gle dogs was setup in which cylindrical
rods of BR and PLLA (as a control) were
implanted into holes drilled in the ani-
mals’ legs. Bone integration was stud-
ied at set time frames up to 24 months
after surgery
[5]
.
As expected, PLLA rods exhibited
little to no absorption at three and
10 months; at 18 months, absorptive
changes were graded as minor to mod-
erate. At 24 months, the absorption
profile of all eight implants was still
graded as moderate.
The BR rods were also fully
intact at three months, but exhibited
minor absorption characteristics at 10
months. By 15 months post-op, the rods
had significant fissures throughout,
although the majority of the BR was
still present. At 18 months, the BR rods
were mostly absorbed and replaced
by a combination of new bone at the
periphery and a mixture of macro-
phages andmesenchymal cells near the
center. By 24 months, the BR material
was 97-99% absorbed
[5]
. This volume
was completely filled with new bone
in four cases and 75-87% filled with
new bone in the remaining four cases
(Fig. 6). Newly formed bone was visu-
ally normal in all respects. This study
provided direct in vivo evidence of
the biocompatibility and appropriate
absorption profile for this material
[5]
.
SUMMARY OF CLINICAL DATA
Following the launch of the first
orthopedic implant made of BR in 2004,
multiple clinical series describing the
osteoconductivity of this material have
been published in the peer-reviewed
orthopedic sports medicine literature,
including at least four in the past three
years
[6-9]
. In total for these studies, 167
patients were followed for between two
and three years after either ACL recon-
struction, repair of Bankart lesions fol-
lowing shoulder instability, or rotator
cuff repair surgery. Radiographic and
magnetic resonance imaging (MRI)
evidence suggest that BR is nearly
Fig. 2 —
Scanning electron micrograph of
Biocryl Rapide (270x).
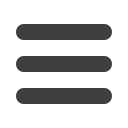
Fig. 3 —
Suture anchors injection molded
fromBiocryl Rapide loaded onto stainless
steel inserters.
Fig. 4 —
Relative pull-out strength of similar suture anchors made of Biocryl Rapide (left), PEEK
(middle), and 6Al-4V titanium (right).
Anchor Pull-Out Strength, N
BR PEEK Ti
400
300
200
100
0
Load, N