A D V A N C E D
M A T E R I A L S
&
P R O C E S S E S | J U L Y / A U G U S T
2 0 1 6
1 9
TECHNICAL SPOTLIGHT
BIOCOMPOSITE MATERIALS
FOR ORTHOPEDIC SPORTS
MEDICINE IMPLANTS
The fourth
—
and most recent
—
step in the evolutionary ladder of materials
for orthopedic sports medicine applications involves composites
made of one or more bioabsorbable polymers.
O
ne of the most important aspects
of orthopedic sports medicine is
attaching soft tissues such as ten-
dons and ligaments to bone. This attach-
ment process is facilitated by a wide
variety of implants in the formof anchors,
buttons, pins, staples, and screws.
Mechanical strength and biocompati-
bility are important properties of these
devices and early generations of implants
weremade frommetal alloys suchasNiti-
nol and stainless steel or plastics such as
polyether ether ketone (PEEK). Potential
disadvantages of these materials include
interference with some imaging modali-
ties, metal sensitivity, and difficulty with
device removal
[1]
.
In the 1990s, bioabsorbable
homopolymers such as poly-L-lactic
acid (PLLA) and polyglycolic acid (PGA)
were introduced. Unfortunately, when
used in isolation, the former material
tends to have a very long degradation
rate, while the latter degrades so rap-
idly that cysts or draining sinuses can
form
[2]
. The patient’s conflicting prior-
ities between implant absorption in
a reasonably short time and avoiding
soft tissue irritation require a delicate
balance from designers of new mate-
rials for sports medicine implants.
Polymer degradation naturally occurs
in the human body as these acids are
incorporated in the tricarboxylic acid
cycle (Krebs cycle) and are ultimately
excreted from the body as carbon diox-
ide and water
[3]
.
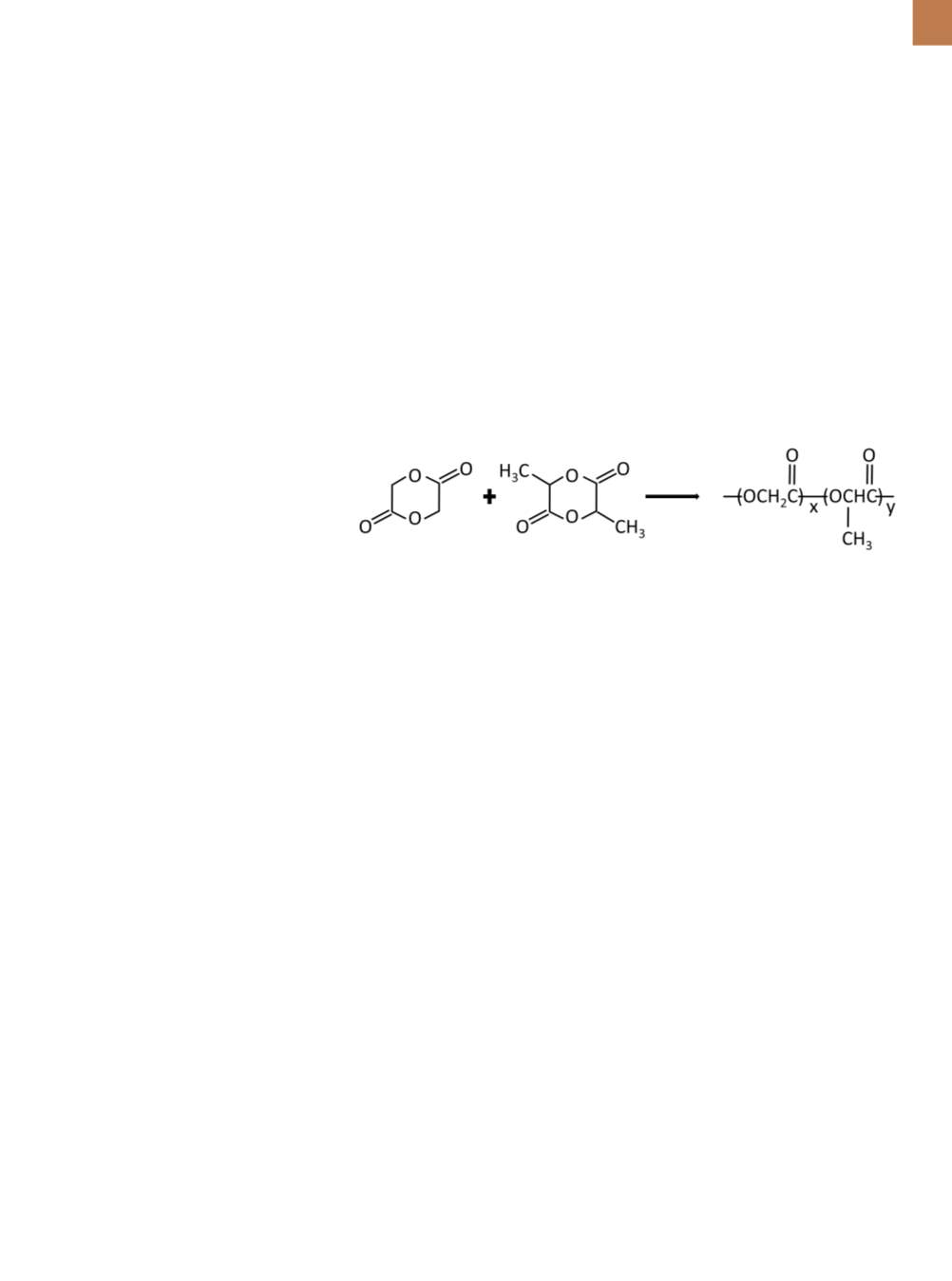
A third generation of implants
uses copolymers of these and other
polymers, as well as stereoisomers of
polylactic acid (PLA) such as combina-
tions of dextro and levo monomers. For
example, L-lactide and glycolide can
be combined to form poly(lactide-co-
glycolide) polymer (PLGA) (Figure 1).
These implants degrade at a sufficiently
fast, but not overly rapid, rate. How-
ever, bioabsorption of the implant does
not typically fill back in with bone, thus
leaving an undesirable area of weak-
ness (i.e., a cavity) in the patient
[4]
.
The fourth—andmost recent—step
in the evolutionary ladder of materials
for orthopedic sports medicine appli-
cations uses composites made of one
or more bioabsorbable polymers with
osteoconductive (bone forming) bioce-
ramics such as
β
-tricalcium phosphate
(
β
-TCP). Extensive preclinical and clini-
cal data exist for one specific formula-
tion comprising 30%
β
-TCP by weight
and 70% PLGA, called Biocryl Rapide
(BR) from DePuy Synthes, Mitek Sports
Medicine, Raynham, Mass. A variety
of implants manufactured from this
material are available including inter-
ference screws for use in anterior cruci-
ate ligament (ACL) reconstructions and
suture anchors for use in both rotator
cuff and labrum repairs in the shoul-
der. All of these surgical procedures are
common in sports medicine.
MANUFACTURING OF
BIOCRYL RAPIDE
Powdered
β
–TCP and PLGA are
dried and then mixed together using
an extrusion machine: The PLGA is
melted and then
β
–TCP is mixed into
the melt using a proprietary micropar-
ticle dispersion process. This technique
ensures homogenous dispersion of the
composite materials (Fig. 2), thereby
reducing the incidence of stress risers
within the implant itself and ensuring
that the osteoconductive
β
-TCP is in
close apposition with the surrounding
bone tissues during the entire absorp-
tion process. The molten composite
exits the machine and is then cut into
pellets approximately 3 mm long. Pel-
lets are later fed into injection molding
machinery to mold specific implants
Fig. 1 —
Chemical structures of L-lactide and glycolide combine to formpoly(lactide-co-
glycolide) polymer (PLGA).